Africa’s male circumcision programs exceed targets, grow more efficient « Blog 4 Global HealthAfrica’s male circumcision programs exceed targets, grow more efficient
This is a guest blog by Meredith Mazzotta of Science Speaks, the blog of the Center for Global Health Policy.
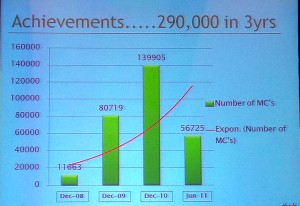
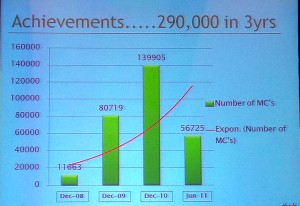
ROME — Kenya, the leader by far in the medical male circumcision (MMC) campaigns underway in sub-Saharan Africa, has successfully serviced 290,000 men and adolescents in the past 2.9 years. This update came from Dr. Peter Cherutich from the National AIDS and Sexually Transmitted Infections Control Program in Kenya, at a satellite session entitled “The Cutting Edge: What’s New in Male Circumcision,” Sunday evening preceding the 2011 International AIDS Meeting in Rome.
Provision of MCC services in Kenya
Randomized controlled trials have shown MMC to protect males from acquiring HIV via vaginal sex by as much as 60 percent.
The majority of MMC has taken place in Kenya’s Nyanza province, which has an HIV prevalence of 48.8 percent and the lowest rate of MMC in the country. Starting with a goal of performing 176,500 circumcisions, nearly 262,000 men have now been circumcised. Exceeding that goal in some part was attributable to underestimating the need and demand for the service in Nyanza, Cherutich said.
“We are now concentrating on the Rift Valley, Western and Nairobi,” he said, where the dynamics of mobilizing partners, getting funding and other issues have drawn out the scale up process. “But soon you will see those numbers coming up very significantly.”
By the end of the campaign, Kenya aims to have circumcised a total of 350,000 men and adolescents. But MMC services in Kenya have also helped to identify HIV infected persons and refer them to treatment and care. Thirty percent of those accessing services were being tested for HIV for the first time, Cherutich said. Assuming a two percent HIV prevalence, 6,000 new cases of HIV have been identified, and 43 cases of other sexually transmitted infections were identified via symptomatic assessment among the more than 55,000 MMC participants in 2010.
Moreover, thanks to exploring procedural efficiencies such as task shifting to use the doctors’ time most effectively, the cost per MMC has dropped almost 50 percent since the program’s inception, Cherutich said, starting out at nearly $50 per circumcision and now down to about $27 per procedure. And the dedicated public health sector workers and nurses in Kenya have been found capable of performing circumcisions just as safely as doctors, he said.

Dr. Peter Cherutich
Key to the program’s success, Cherutich said, is the support the MMC campaign receives from political leaders in the country, encouraging donors and helping to generate demand for services. Fellow panelist Catherine Hankins from UNAIDS noted that the king of Swaziland announced Saturday a dramatic large-scale initiative to circumcise adult and adolescent males in his country, reversing a declaration of the previous Swazi king who had forbidden the practice.
“When that kind of leadership happens, then people feel they can do this, “ Hankins said.
Generating demand for services has been particularly challenging for Kenya’s neighbor to the south, according to Jhpiego’s Hally R. Mahler.
But they are creatively working to match supply with demand. After a slow start to the program in 2009, the MMC program in the Iringa province streamlined services – utilizing more efficient surgical techniques (the forceps-guided method), prepping multiple surgical bays, task sharing, etcetera – and in February set out to circumcise 6,000 men and adolescents in six weeks at five facilities. They formed demand creation committees in each district, asked their U.S. government partners in the region to help support MMC by restructuring activities, and developed print, radio and loud speaker ads to promote MMC in the community.
“Actually the thing that got the most clients was a car with a loud speaker that drives around to get clients,” Mahler said. “You could drop everything else and just do that and be just fine in Tanzania.”
By decongesting service delivery sites by adding tents and other temporary structures for the voluntary counseling and testing (VCT) part of the MMC service package, advance-scheduling clients, and adding additional VCT counselors, the campaign successfully kept up with the increase in demand for services. To motivate the over-worked doctors, Mahler said, they would count the number of MMCs performed and calculate the number of HIV infections averted knowing that for every 4.5 people circumcised in Tanzania, one infection is averted.
“As a result we did 10,352 circumcisions in six weeks at these five sites… we far exceeded our goal,” Mahler said, adding that overall more than 100,000 MMCs have been performed in Tanzania since this time last year.
“The Tanzania program is not particularly well funded at the moment, we don’t have as much money as we would like to have,” Mahler said, “[but] efficiencies have really helped us to be cost effective.”
She noted some challenges the program has faced so far that they are working to address, including how to get older men to circumcise, adult men not wanting to be circumcised in the same area as younger clients, and stigma related to getting circumcised after having fathered a child. Mahler said they hope to publish a paper on these observations soon.